Volume: 56 Issue: 2 - 2022
| 1. | Cover Pages I - IX |
| ORIGINAL INVESTIGATION | |
| 2. | Perceptions and knowledge toward cosmetic procedures: A cross-sectional survey Vildan Manav, Dilara İlhan, Elif Bal Avcı, Asude Kara Polat, Duygu Erdil, Soysal Baş, Ayşe Esra Koku Aksu doi: 10.4274/turkderm.galenos.2021.66563 Pages 51 - 57 Background and Design: Cosmetic procedures have been increasing recently, and public knowledge on this issue is made available through the internet, television, or social media. However, with the increasing tendency for these procedures, the risk of complications also increases because of practitioners who do not have expertise in this field. This study aimed to determine the perceptions and knowledge toward cosmetic procedures and its complications. Materials and Methods: A total of 324 patients aged 18 years and over presented to the cosmetology outpatient clinic. Results: The majority of the participants stated that dermatologists and/or plastic surgeons are the most qualified to perform cosmetic procedures (77.2%). Particularly, female participants and the high-income group answered that they will choose dermatologists and plastic surgeons for performing cosmetic procedures (p=0.028 and p=0.010, respectively). Conclusion: While most of the participants perceived that these procedures are performed by dermatologists or plastic surgeons, cosmetic procedures are performed in the skin care center by non-healthcare providers because of socio-economic reasons. However, if complications occur, patients first sought dermatologists for treatment. Therefore, society should be more conscious of this issue when planning to undergo cosmetic procedures by experts and to prevent complications. |
| 3. | Efficacy of intralesional tranexamic acid in melasma: Assessment with Melasma Area Severity Index and Dermatology Quality of Life Index Sneha Krishnoji Rao, Rajashekar T. S., Ashna Ashraf doi: 10.4274/turkderm.galenos.2022.42709 Pages 58 - 63 Background and Design: Melasma is a common hypermelanotic condition, mostly observed in women, which affects their psychological, emotional, and social well-being as well as their quality of life. Although melasma is relatively resistant to treatment, various therapeutic options have been attempted until date. Recently, microneedling and microinjection tranexamic acid were performed. To compare the therapeutic effectiveness of triple combination therapy with tranexamic acid injection and assess the impact of response on melasma by comparing the pre- and post-treatment Melasma Area Severity Index (MASI) and Dermatology Quality of Life Index (DLQI) scores. Materials and Methods: A total of 70 melasma patients were selected and assigned to two groups of 35 patients each based on the interventional randomized control study. One group was treated with a topical triple combination therapy-hydroquinone (2%), mometasone (0.1%), and tretinoin (0.025%), and the other group with injectable tranexamic acid. The MASI scores and DLQI were assessed for both the groups of patients at the baseline and then 6 weeks later along with serial photographs. Results: Significant reduction in MASI and DLQI scores were noted in the intralesional tranexamic acid group of patients (p=0.032). The mean change in MASI with tranexamic acid was 1.22 and with DLQI was 2.03. Conclusion: Injectable tranexamic acid is a promising treatment option for melasma. Further studies are however warranted with a larger sample size and for a longer duration to determine its long-term benefits. Treatment of melasma is beneficial for the patient both physically and emotionally. |
| 4. | Comparison of the efficacy of microneedling combined with 5-fluorouracil 5% cream versus microneedling combined with tacrolimus 0.1% ointment in the treatment of vitiligo Parwaaz Matharoo, Saurabh Sharma, Jasleen Kaur, Roopam Bassi doi: 10.4274/turkderm.galenos.2022.57804 Pages 64 - 69 Background and Design: Vitiligo is an acquired depigmenting disorder associated with profound psychological effects. It can manifest as depigmented macules that can be localized or generalized in nature. Various morphological types are seen in patients. Despite existing therapeutic options, none is yet proven to be an ideal method for all patients. Materials and Methods: Sixty lesions in 30 patients with vitiligo were divided into two groups and subjected to microneedling with DermaPen after topical application of 5-fluorouracil (5-FU) cream 5% in one group and tacrolimus ointment 0.1% in another group. This procedure was repeated every 2 weeks for a maximum of 10 sessions. Patients were followed up for 6 months after the last session. Results: The overall repigmentation rate was significantly higher with 5-FU than with tacrolimus. Good-to-excellent response was seen in 76.7% of the lesions with 5-FU and 63.7% of the lesions with tacrolimus. Acral areas showed good-to-excellent response in 50% of the lesions in group A, and in group B, good response was seen in 50% lesions, whereas none attained excellent improvement. Conclusion: Microneedling with 5-FU and tacrolimus appears to be safe and effective therapeutic intervention for stable refractory vitiligo. Both combinations were tolerated well, but 5-FU demonstrated significantly quicker and higher response. |
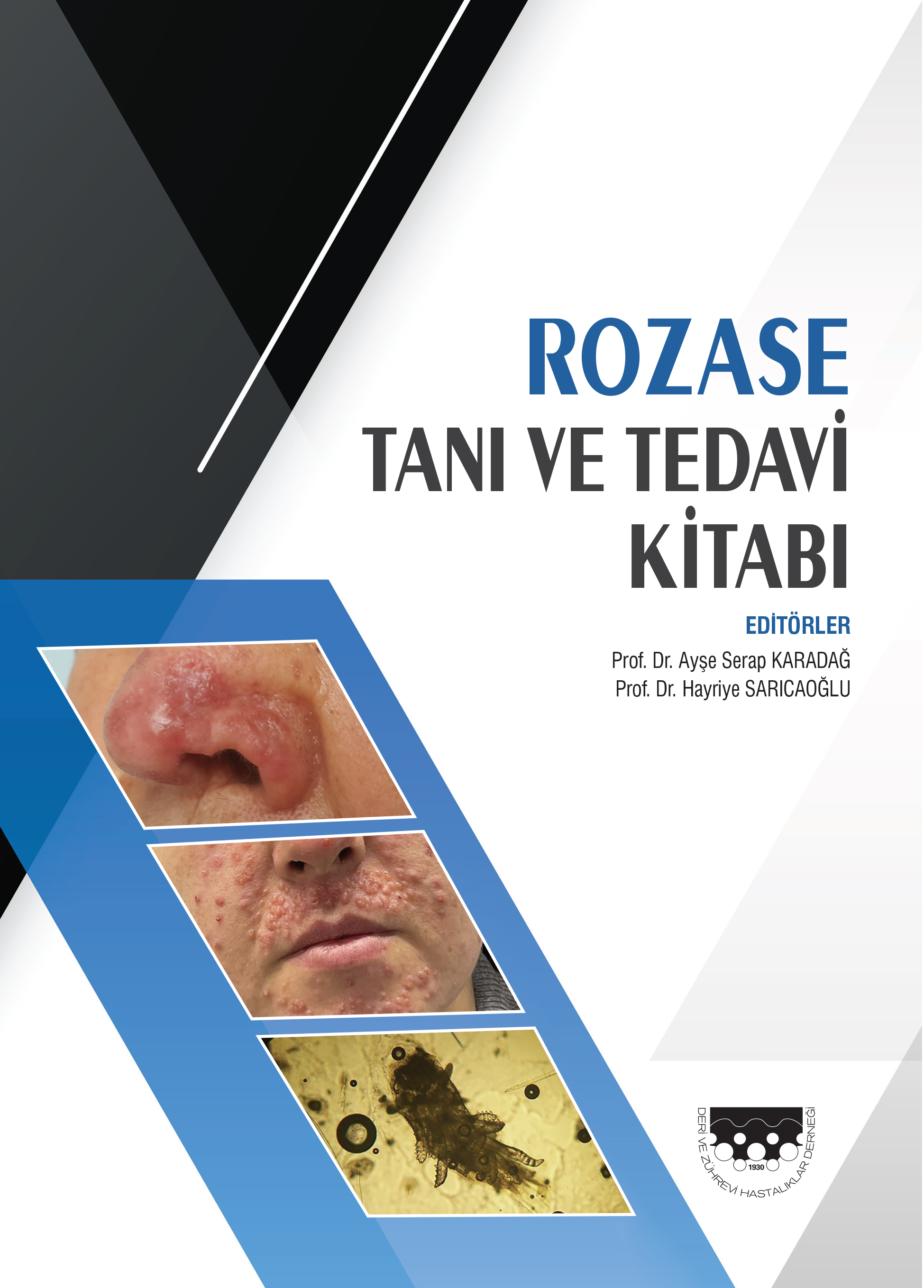
| 5. | Evaluation of the incidence of Demodex in eyelashes in rosacea patients with ocular involvement Zuhal Metin, Nermin Boyraz, Firdevs Örnek, Evin Şingar Özdemir, Hatice Meral Ekşioğlu doi: 10.4274/turkderm.galenos.2022.44788 Pages 70 - 75 Background and Design: Demodex, a mite, is known to influence the etiopathogenesis of rosacea, pityriasis folliculorum, pustular folliculitis, perioral granulomatous dermatitis, hyperpigmented patch, and chronic blepharitis. This study aimed to investigate the relationship between Demodex, which is increasingly important in the pathogenesis of rosacea, and ocular rosacea. Materials and Methods: A total of 103 rosacea patients with ocular involvement (ocular rosacea) and 140 volunteers without facial dermatosis were included in the study as the control group. Written and verbal consent was obtained from the participants. A total of five eyelashes were pulled from the upper and lower eyelids of one or both eyes of the patient group and control group, using forceps, and the presence of Demodex was examined by the epilation method and standard superficial skin biopsy method from the face. Under a light microscope, ≥1 and ≥5 Demodex per cm2 in the eyelashes and face were evaluated as positive, respectively. Results: Of the 103 patients, 27 (26.2%) had conjunctivitis, 77 (74.8%) had blepharitis, 1 (1%) had hordeolum, and 24 (23.3%) had meibomian gland dysfunction. The eye examination findings of the control group were normal. The Demodex incidence rates were 84.5% and 29.3% in the patient group and control group, respectively. Of the 103 patients with rosacea accompanied by ocular rosacea, Demodex mites were present in the eyelashes and face of 51 patients (49.6%), only in the eyelashes in 26 (25.2%), and only in the face in 10 (9.7%). No Demodex mites were present on both eyelashes and face in 16 (15.5%) patients. Conclusion: The results of this study show that Demodex positivity was detected at a higher rate in the eyelashes and face in patients with rosacea compared with the controls. Demodex may play an important role in the pathogenesis of rosacea and ocular rosacea. |
| 6. | Juvenile unilesional folliculotropic mycosis fungoides: Two siblings with HLA-DRB1*04 and HLA-DQB1*03 alleles Hatice Şanlı, İncilay Kalay Yıldızhan, Bengü Nisa Akay, Canan Arı, Aylin Okçu Heper doi: 10.4274/turkderm.galenos.2022.89083 Pages 76 - 79 The pathogenesis of mycosis fungoides (MF) is poorly understood, and an immunogenetic mechanism has been suggested to play a role. Human leukocyte antigen (HLA) class II alleles DRB1*11 and DQB1*03 were found to be significantly increased for patients with sporadic and/ or familial MF. The juvenile-onset familial MF is extremely rare. Herein, we report two siblings diagnosed with folliculotropic MF, both exhibiting similar morphology of a unilesional presentation on the flexural region of the arms. Both were positive for HLA-DRB1*04 and HLA-DQB1*03 alleles. The HLA-DQB1*03 allele has been described in familial MF in the literature recently, whereas HLA-DRB1*04 allele has not been reported previously in familial MF cases. |
| CASE REPORT | |
| 7. | Pemphigus vulgaris in a patient with primary hypogammaglobulinemia: A case report Uğur Hacı Musabak, Tuba Erdoğan, Mustafa Tunca doi: 10.4274/turkderm.galenos.2022.81370 Pages 80 - 83 Pemphigus vulgaris (PV) is a rare autoimmune disorder characterized by blisters on the mucous membranes and skin. Autoimmunity is an important complication developing in predominantly antibody deficiencies, which is a subgroup of primary immunodeficiencies (PID). Herein, we present a patient with PV who had primary antibody deficiency and whose disease relapsed during the maintenance period of conventional immunosuppressive treatments but progressed to remission following high-dose intravenous immunoglobulin therapy. Thus, we aimed to create awareness for the study of primary immunodeficiencies in rare autoimmune bullous diseases. |
| 8. | Macrophage activation syndrome due to juvenile amyopathic dermatomyositis with atypical onset Esma İnan Yüksel, Betül Demir, Metin kaya Gürgöze, Ilknur Calik doi: 10.4274/turkderm.galenos.2022.72368 Pages 84 - 87 Macrophage activation syndrome (MAS) is a life-threatening condition associated with rheumatic diseases. It is rarely reported in juvenile dermatomyositis. An 8-year-old girl was admitted with complaints of joint swelling and psoriasiform plaques on the elbows. She was diagnosed with psoriatic arthritis, and methotrexate therapy was started. Three months later, she was readmitted with fever, fatigue, and weight loss. Hepatosplenomegaly was found on physical examination. The muscle strengths were 5/5. Dermatological examination revealed facial edema, widespread maculoerythematous rash, and xerosis. Erythematous-violaceous papulosquamous plaques were seen on the dorsal surfaces of the elbows and metacarpophalangeal and proximal interphalangeal joints. Based on the clinical and laboratory findings, the patient was considered to have MAS secondary to juvenile amyopathic dermatomyositis (JADM). The cutaneous manifestations seen in MAS are not specific but depend on the underlying rheumatic disease. Given the atypical onset, this was considered a case of JADM misdiagnosed as psoriasis, which rapidly progressed to MAS. |
| 9. | Lichen planus occuring after Coronavirus disease-2019: A case report Zuhal Metin, Koray Durmaz, Deniz Unluer Kapiskay doi: 10.4274/turkderm.galenos.2022.24571 Pages 88 - 90 The novel Coronavirus disease-2019 (COVID-19), which emerged in December 2019 and caused an unexplained viral pneumonia, rapidly spread worldwide within a few months. A pandemic was declared by the World Health Organization in March 2020. Several cutaneous manifestations of the disease among patients with COVID-19 have been reported. Thus far, the most frequently reported cutaneous findings are morbiliform rash, urticarial lesions, purpuric lesions, oral vesicles, and pityriasis rosea. This report presents a case of lichen planus secondary to COVID-19 and its histopathological findings, which is rarely reported in the literature. |
| WHAT IS YOUR DIAGNOSIS? | |
| 10. | What is your diagnosis? Rosanne Ottevanger, Roel E. Genders doi: 10.4274/turkderm.galenos.2022.14412 Pages 91 - 92 not applicable |