Volume: 54 Issue: 4 - 2020
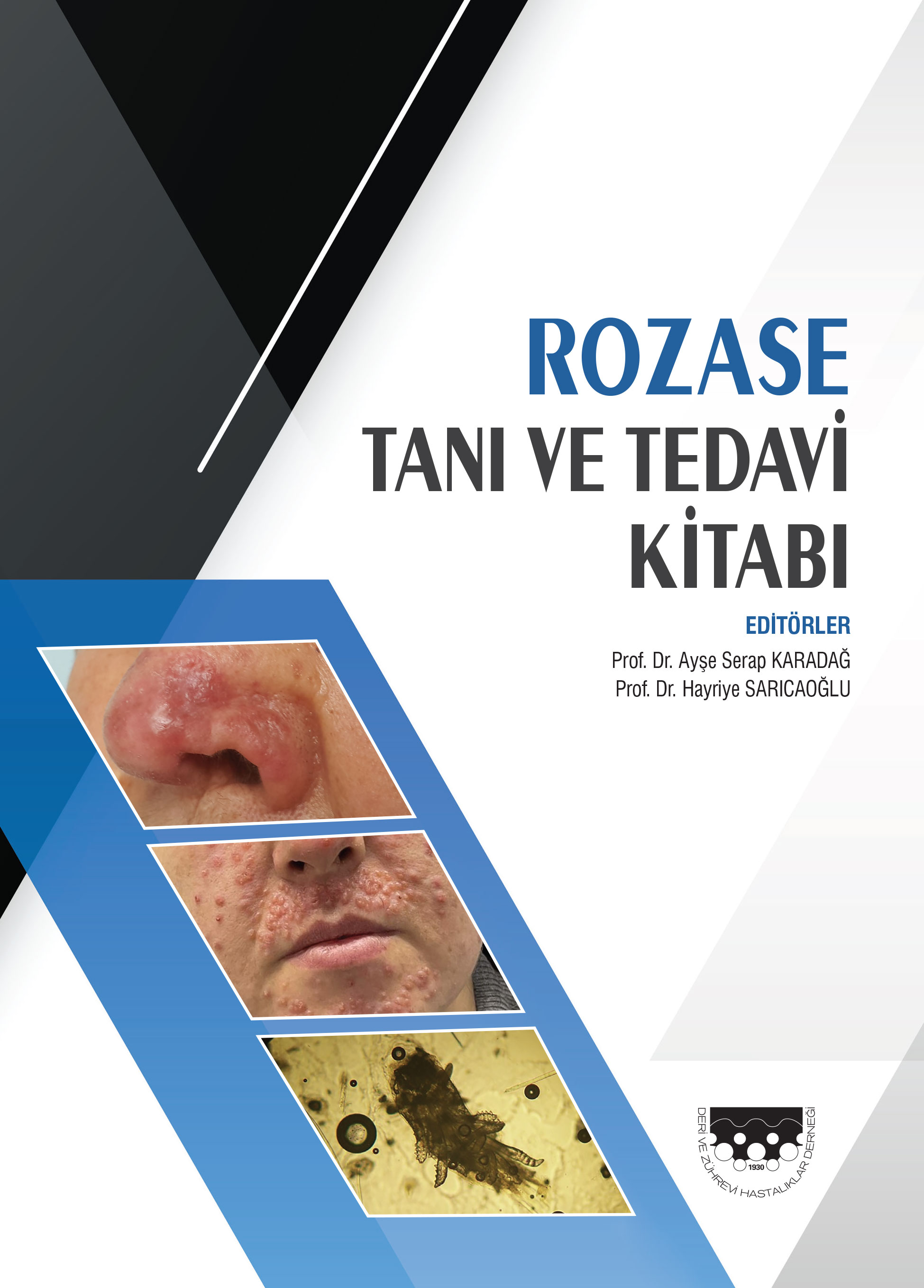
| 1. | Cover Pages I - VI |
| ORIGINAL INVESTIGATION | |
| 2. | Information about sun exposure, protection, awareness and behavioural patterns of medical students in Kolar Shruthi Madhavi Govindarajulu, Rajashekar Taları Srinivas, Suresh Kumar Kuppuswamy, Priya Prem doi: 10.4274/turkderm.galenos.2020.38455 Pages 124 - 131 Background and Design: The harmful ultraviolet radiation of sunlight can damage skin cells and affect the skins normal appearance. The short term effects associated with sun exposure include acute skin damage associated changes such as sunburn, suntan and the long term effects are delayed pigmentation, impaired vitamin D synthesis, altered immunological responses of the skin, photodamage and photocarcinogenesis. The majority of these photodermatoses are preventable with the implementation of appropriate sun protection measures and behavioral changes. Materials and Methods: Data collection was done with the help of a structured questionnaire which was distributed among 339 undergraduate medical students in their 4th, 7th, 8th and 9th term attending dermatology postings at a medical college attached to a tertiary hospital from January 2018 to July 2018. Results: The majority of the students in this study were 4th term undergraduates representing 35.3% of the population. The mean ± standard deviation scores of knowledge, behaviour and awareness were 11.67±3.31, 12.32±5.004, 24±6.282, respectively. Only 26.8% of the above population always used sunscreen during daily activities, 32.1% sometimes, 25.6% rarely used and 15.3% never used sunscreen during daily activities. One-Way ANOVA tests depicted a statistically significant difference among the various term students with respect to variables of knowledge, behaviour and awareness score with a p<0.001. Conclusion: The results of this study indicate that knowledge regarding sun exposure and its adverse effects, behaviour and awareness even among medical students to sun protection is inadequate. Sun protection should start at an early age and therefore awareness campaigns are highly recommended. |
| 3. | Effect of isotretinoin on periodontal tissues and oxidative stress markers in the saliva Gülbahar Ustaoğlu, Şevki Güler, Mualla Polat doi: 10.4274/turkderm.galenos.2020.99896 Pages 132 - 137 Background and Design: Isotretinoin is a vitamin A isomer, and is the most commonly used drug for the treatment and for achieving remission in severe acne. This study aimed to evaluate the effects of isotretinoin on periodontal tissues by assessing the clinical periodontal parameters and salivary oxidative stress (OS) markers. Materials and Methods: Twenty-five patients (17 women and 8 men) aged between 20 to 25 years old, who were identified as candidates for the treatment of acne with isotretinoin; and 18 healthy volunteers (14 women and 4 men), who were age- and sex-matched with the patients, and who did not have any inflammatory skin diseases or periodontal diseases, were included in the study. Patients received isotretinoin after their clinical periodontal parameters were recorded and saliva was collected at the baseline. Clinical periodontal parameters and salivary oxidative biomarkers were evaluated before and after 6 months of isotretinoin treatment. Results: The baseline periodontal clinical parameters and salivary biomarkers were not statistically different between groups (p>0.05). The total antioxidant capacity (TAC) values of the patient group were found out to be statistically decreased in the sixth month compared to the baseline (p=0.001). Conclusion: The study demonstrated that the use of isotretinoin due to acne vulgaris did not create significant changes in the periodontal tissues, but caused a significant decrease in the TAC levels. These alterations in the OS regulation may potentially take part in the pathological mechanisms involved in the emergence of isotretinoins adverse effects. |
| 4. | Evaluation of serum vitamin D levels in patients with lichen planus Deniz Aksu Arıca, Leyla Baykal Selçuk, Asım Örem, Zeynep Karaca Ural, Savaş Yaylı, Sevgi Bahadır doi: 10.4274/turkderm.galenos.2020.66664 Pages 138 - 142 Background and Design: Lichen planus (LP) is a chronic inflammatory disease of unknown etiology that most commonly affects the skin and oral mucosa. Vitamin D is a steroid hormone with immunomodulatory, anti-inflammatory and antioxidant effects. The purpose of this study was to evaluate serum vitamin D levels in patients with LP and to compare these with those of healthy control subjects. Materials and Methods: Forty-eight patients with a diagnosis of LP and 46 healthy controls were enrolled in the study. The serum levels of 25-hydroxy vitamin D, calcium, phosphate and parathyroid hormone were studied from blood samples collected from all subjects. Results: The serum levels of vitamin D were lower in the LP patients compared to the controls and in the oral erosive LP patients compared to the other LP patients, although the difference was not statistically significant. There were no statistically significant differences in other laboratory parameters between the patient and the control groups. Conclusion: Our study revealed no clear relation between LP and vitamin D levels. The results of our study suggest that other factors except vitamin D, particularly probable triggers, play a more dominant role in the immunopathogenesis of LP. Further studies with larger patient populations assessing serum vitamin D levels in different types of LP and vitamin D-related gene polymorphisms are now needed in order to reveal the relation between LP and Vitamin D more clearly. |
| 5. | The use of an urticaria control test for the evaluation of omalizumab treatment response in patients diagnosed with chronic urticaria Burhan Engin, Sera Nur Yücesoy, Özge Aşkın, Zekayi Kutlubay, Server Serdaroğlu doi: 10.4274/turkderm.galenos.2020.06887 Pages 143 - 147 Background and Design: Urticaria is a very common skin disease which is characterized by itchy, erythematous and edematous plaques. Angioedema can also be seen in half of the cases in addition to skin findings. In most cases of chronic urticaria, the underlying factor is not known. Omalizumab, a recombinant human monoclonal immunoglobulin G (IgG) antibody against IgE, is a safe treatment option in chronic urticaria cases which are resistant to treatment with antihistamines. This study aimed to evaluate the treatment responses of chronic urticaria patients taking omalizumab treatment with an urticaria control test (UCT). Materials and Methods: One hundred fifty-four patients diagnosed with chronic urticaria taking omalizumab treatment attended our evaluation between January 1, 2017 and December 31, 2018. These patients were evaluated with an UCT every four weeks. Sixty-six patients who were evaluated with an UCT during the course of the following 12 weeks were statistically analyzed. Thirty-nine of the patients received a treatment shorter than 12 months (the first group), and the remaining 27 patients received treatment for longer than 12 months (the second group). The patients were analyzed according to the duration of their treatment. Results: The first, second, and third average UCT scores of the 3 sequential applications for the first group were 9.16; 11.57; and 12.73; respectively. There was a statistically significant difference in the UCT scores between the 3 successive applications in the first group (p<0.05). On the other hand, the first, second, and third average UCT scores of the 3 sequential applications for the the second group were 11.20; 11.40; and 12.36 respectively. There was statistically significant difference in the UCT scores between the 3 successive applications for the second group. Conclusion: The effectiveness of omalizumab treatment in chronic urticaria patients with an UCT was investigated in this study. Omalizumab proved to be an effective treatment option in chronic urticaria patients. |
| 6. | The frequency of epicardial fat pads detected by chest x-rays in psoriasis patients Sibel Doğan, Pelin Esme, Meltem Gülsün Akpınar, Nilgun Atakan doi: 10.4274/turkderm.galenos.2020.74240 Pages 148 - 151 Background and Design: Psoriasis is a chronic inflammatory skin condition associated with several systemic comorbidities including cardiovascular diseases (CVD). Epicardial fat pad (EFP) is defined as a visceral fat tissue surrounding the heart and coronary vessels. Recent studies revealed epicardial fat thickness, which is also increased in psoriasis, as an early sign of CVD. The aim of this study was to evaluate EFP prevalence and its associations in psoriasis patients. Materials and Methods: Two hundred thirty-seven psoriasis and 113 control patients were assessed for CVD risk factors, Psoriasis Area Severity Index, body composition parameters and laboratory work-up. Controls were chosen from outpatients who lack any chronic inflammatory skin disease and/or systemic inflammatory disease. Evaluation of chest X-rays were performed by a radiologist who was unaware of clinical data. Results: 42.2% of psoriasis patients (n=100) and 31% of controls (n=35) had EFP detected on chest X-ray revealing psoriasis patients had significantly more prevalent EFP than the controls (p=0.047). Prevalence of major CVD risk factors was statistically higher in psoriasis patients (60%, n=142) compared to controls (32%, n=36), (p<0.01). Psoriasis patients with EFP presented higher prevalence of CVD risk factors (70%, 4, n=69) compared to patients who did not have EFP (53%, n=67) (p=0.009). Conclusion: EFP is associated with concurrent CVD risk factors and is more prevalent in psoriasis. It can be detected by a first-line imaging method like chest X-ray which is quite cheap, easy to perform and applicable to almost each patient. |
| CASE REPORT | |
| 7. | Acute generalized exanthematous pustulosis caused by a probable spider bite: A case report and review of the literature Fatmagül Dirican, Ayda Acar, Banu Yaman, Bengü Gerçeker Türk doi: 10.4274/turkderm.galenos.2020.30906 Pages 152 - 155 Acute generalized exanthematous pustulosis (AGEP) is a toxic cutaneous reaction pattern that is mostly caused by drug intake and rarely associated with spider bites. We report a case of a female patient, 47 years old, with febrile pustular lesions on an erythematous base at the abdominal region. She had three violaceous erythematous and edematous plaques on the interscapular region, one of which had a necrotic crust at its center. The lesions were compatible with spider bites. By considering histopathological and clinical findings, the patient was diagnosed with AGEP. Since she had no history of drug intake, viral infection or other triggers, a spider bite was thought to have caused the AGEP |
| 8. | Fluoroscopy-induced chronic radiation dermatitis treated with excision and reconstructed with rhomboid flap Müge Göre Karaali, Soner Karaali, Ayşe Esra Koku Aksu, Mehmet Salih Gürel doi: 10.4274/turkderm.galenos.2020.26918 Pages 156 - 158 Fluoroscopy is widely used for minimally invasive procedures. The diagnosis of fluoroscopy-induced chronic radiation dermatitis (FICRD) may be overlooked, because patients may unintentionally be exposed to radiation in surgical procedures. Prolonged or multiple procedures increase the risk of acute and chronic skin damage. Herein, we report a patient diagnosed with FICRD treated with excision and reconstructed with rhomboid flap. Due to the risk of radiation-related malignancy, complete surgical excision and suitable reconstruction according to the skin defect may be preferred as a treatment option. Clinical follow-up is important especially following prolonged fluoroscopy-guided procedures. |
| 9. | A case of temporal triangular alopecia Emre Zekey, Gülcan Saylam Kurtipek doi: 10.4274/turkderm.galenos.2020.56578 Pages 159 - 161 Temporal triangular alopecia (TTA) is a non-cicatricial alopecia characterized by an alopecic patch, usually located in the frontotemporal region, unilateral or bilateral, with an oval or narrow triangular base and no terminal hairs on it. It can manifest at birth or develop in the first years of life. It is a rare condition and its exact etiology remains unknown. The diagnosis is based on its clinical appearance. The differential diagnosis includes alopecia areata, trichotillomania, tractional alopecia and congenital aplasia cutis. Due to its rarity, misdiagnosis and unnecessary treatments can be applied. Clinical and dermoscopic examination is sufficient in the diagnosis of the disease. A 3-year-old boy with a diagnosis of TTA is presented as a case report. |
| 10. | Unexpected temporal localization of tuberculosis verrucosa cutis Selami Aykut Temiz, İlkay Özer, Arzu Ataseven, Recep Dursun, Mustafa Cihat Avunduk doi: 10.4274/turkderm.galenos.2020.68812 Pages 162 - 164 Clinical forms of cutaneous tuberculosis (TB) which is a chronic granulomatous disease, varies by the route of entry into the body, the number of bacilli, its virulence and the immunological response of the body. TB verrucosa cutis (TBVC) occurs in patients who have previously been affected by tuberculosis bacilli with healthy immunity. A 68-year-old male patient was referred to our dermatology outpatient clinic from an external dermatology center with complaint of verrucous plaques on the left temporal region, persisting for two months. After a diagnosis of wart and seborrheic keratosis, cryosurgery and destructive procedures were applied to the lesions of the patient many times. Histopathological examination revealed granulomatous textures classified by infiltration of inflammatory cells around the keratin plugs and giant multinuclear cells in the epithelium sublayer, and positive staining with CD68 was detected in immunohistochemical examination. The patient was diagnosed with TBVC clinically and histopathologically. At the end of the anti-tuberculosis treatment, the lesions largely regressed with postinflammatory hyperpigmentation. Herein, we report a case of TBVC with unusual localization, which was initially misdiagnosed as wart and seborrheic keratosis. This case emphasizes the importance of differential diagnosis |
| LETTER TO THE EDITOR | |
| 11. | Complex aphthosis-like pemphigus vulgaris during pregnancy Sema Aytekin, Fatih Göktay, Şirin Yaşar, Pembegül Güneş doi: 10.4274/turkderm.galenos.2020.17003 Pages 165 - 166 Abstract | |
| DERMOSCOPY FOR ALL DERMATOLOGISTS | |
| 12. | Dermoscopic and reflectance confocal microscopic findings in a case of plasma-cell cheilitis Banu Yaman, Işıl Karaarslan, Ayda Acar, Mine Hekimgil, Taner Akalın, Fezal Özdemir doi: 10.4274/turkderm.galenos.2020.22571 Pages 167 - 169 Abstract | |
| OTHER | |
| 13. | Subject Index Pages E1 - E3 Abstract | |
| 14. | Referee Index Page E4 Abstract | |
| 15. | Author Index Page E5 Abstract | |